SGF presented two new studies during the American Society for Reproductive Medicine’s (ASRM’s) 2018 Scientific Congress in Denver, CO that sought to better understand the known health disparities affecting reproductive outcomes among African American Women.
Study 1: Aimed to Identify Reasons Why African Americans Experience Reduced Pregnancy, Higher Pregnancy Loss and Lower Live Births from IVF Despite Producing More Eggs and Transferring Higher Quality Embryos as Compared to Caucasian Women
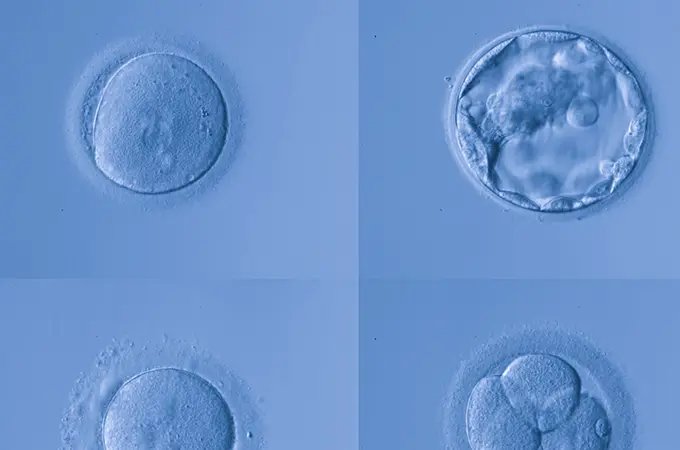
Multiple prior published studies have demonstrated that African-American women experience lower pregnancy rates, higher pregnancy loss, and lower live birth rates from in vitro fertilization (IVF). In this study, SGF evaluated more than 40,000 IVF cycles of more than 22,000 Caucasian and African-American patients to better understand why African-American women experienced poorer IVF outcomes.
What did the findings show?
“Our results suggest that African-American women respond just as well to medications that stimulate egg production, produce as many eggs, and actually produce more good quality embryos than Caucasian patients,” says Dr. Isaac E. Sasson, SGF physician and a key researcher on this study. “However, overall chances of success are decreased among African-American patients. The sum total of these data suggest that uterine factors are the most likely cause of decreased success from IVF among African-American patients,” adds Sasson.
Consistent with prior studies, this study found that birth rates per embryo transfer were 14 percent lower for African-American women compared with Caucasian women as a result of both lower pregnancy rates and higher pregnancy losses.
“The good news is that, armed with this information, African-American women and their physicians can make more informed decisions about their gynecologic and fertility care. Preventive care can help detect potential problems in their earliest, easiest to treat state. Annual OB/GYN annual examinations are critical, as is seeking care early when a woman experiences infertility or recurrent miscarriage. Early treatment leads to much more favorable outcomes,” adds Sasson.
Study 2: Aimed to Identify the Reasons Why African Americans Experience Lower Gestational Age and Increased Risk of Preterm Birth Associated with Singleton Pregnancies from IVF Compared to Caucasian Women
In the second study, researchers set out to identify whether African-American women with singleton IVF pregnancies were more likely than their Caucasian counterparts to experience preterm birth. Prior studies of predominantly naturally conceived pregnancies, have consistently demonstrated that African-American women have a higher risk for preterm delivery, and this has been hypothesized to be largely attributable to decreased access to care. Therefore the investigators set out to determine whether this increased risk was also present in the IVF population, who, by definition, have access to healthcare.
What did the findings show?
“Singleton births among African-American IVF patients occur almost a week earlier, and are three times more likely to be very preterm (28-32 weeks) or extremely preterm (<28 weeks) compared with Caucasians,” says Lauren Bishop, a lead investigator on this study.
“Unfortunately, in addition to lower live birth rates from IVF, African Americans are also more likely to experience preterm birth following IVF, and uterine factors are most likely the cause of both. Fibroids disproportionately affect our African-American population and are likely a major contributor to the poorer outcomes we observed in these two studies. The good news is that armed with this information, we can act as advocates for this patient population and do more research to further evaluate for causes and solutions,” says Dr. Sasson who was also a key researcher on this second study.
What is the biggest takeaway of both of these studies?
Given uterine conditions are more prevalent among African-American women, SGF physicians recommend that when infertility or recurrent pregnancy loss occur, patients should consult with a specialist right away. One in eight couples experience infertility, and SGF strives to reach as many people as possible, since early intervention offers the best chances of success.
Why Research?
We view research as a way of “giving back” to our field as it gives us tremendous insights into the best fertility practices. Our commitment to continual improvement keeps us among the forefront, innovating and refining, which ultimately provides better outcomes—not just the treatment of our patients but of those across the country.
“Research remains one of the key pillars at SGF. It is, after all, the only way we can understand how to provide better treatment, improved care, and more successful results,” says Kevin S. Richter, Ph.D., Research Scientist for Shady Grove Fertility.
To learn more about this study, or to schedule an appointment with one of our physicians, please call our New Patient Center at 888-971-7755 or complete a brief online form.