Medical Contribution by: Shruti Malik, M.D., FACOG
When people think about how weight affects their health, they focus on diseases and disorders. Diabetes, heart disease, and thyroid dysfunction aren’t the only health concerns that can exist though. Physicians have found that body mass index (BMI) can have a profound effect on a person’s fertility. Both men and women can be affected by their BMI when trying to conceive, whether they are underweight or overweight. For some, BMI might even be the cause of their infertility, which has led Shady Grove Fertility to increase patient education about the role that weight plays in trying to conceive. The following facts can help patients better understand how their BMI is affecting their fertility and what they can do to improve their chances of conception – as well as their own health.
What is the ideal BMI if I’m trying to conceive?

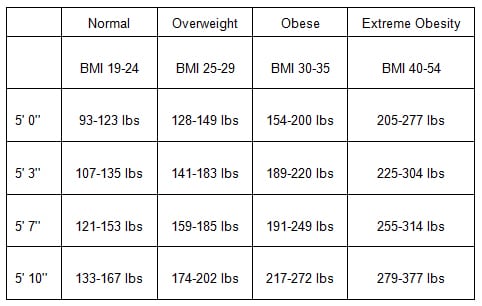
Body mass index (BMI) is a measure of your body fat based on height and weight. This measurement allows physicians to determine what sizes constitute being underweight, overweight, obese, or extremely obese. A normal (or “ideal”) BMI falls between 19 and 25. While women can be under or overweight and still conceive, the ideal BMI is what is recommended for a healthy pregnancy for both mother and baby.
- Want to discover your BMI? Use the National Institute of Health’s (NIH) online BMI calculator.
BMI Weight Conversion Table
How is fertility affected by BMI?
A woman’s BMI is strongly connected to her fertility potential. While not every woman who is underweight, overweight, or obese will have difficulty conceiving, there are many that do. “Epidemiological data confirms that obesity accounts for the primary cause of infertility in 6% of infertility patients; additionally, low body weight in women also accounts for the primary cause of infertility in another 6% of patients [1],” says Shruti Malik, M.D., of Shady Grove Fertility’s Fair Oaks, VA office.
Weight becomes an issue at the very outset for some women due to ovulatory dysfunction. Women who are underweight are not getting enough nutrients, which can cause their bodies to ovulate infrequently or not at all. In overweight women, an increase in insulin levels may cause the ovaries to reproduce male hormones and stop releasing eggs. In both instances, ovulatory dysfunction can make conception very difficult.
In many women with a BMI that is above or below normal, diet, exercise, and lifestyle changes have been shown to make a significant difference in a woman’s fertility potential. In patients whose infertility is specifically due to weight, correction of the underlying disorder will lead to spontaneous conception in up to 70% of women [2]. Underweight patients who bring their weight up to the ideal level, and overweight patients who undergo significant weight loss, can often (though not always) begin to ovulate again. Studies have shown that losing as little as five-ten percent of body weight can dramatically improve the chances of pregnancy occurring [3].
Does BMI affect fertility treatment success rates?
While some women can gain or lose weight to achieve the ideal BMI for conception, this is not the case for everyone. Many patients will enter treatment when they are overweight (see “Do fertility centers have BMI restrictions for patients who need to undergo treatment?” below to find out SGF’s weight guidelines for treatment). Additionally, some patients have more factors affecting their fertility than just weight, making fertility treatment necessary irrespective of weight gain or loss.
For under or overweight patients, BMI can affect treatment as early as the stimulation phase. Women with a higher BMI are typically seen to have a lower response to medication used to regulate or initiate ovulation, which can lead to cancelled cycles.
“When women are under or overweight, their BMI has been found to impair successful outcomes for in vitro fertilization (IVF) cycles. During the egg retrieval procedure, it can be technically difficult to reach the patient’s eggs, so that consequently, chances of conception are decreased. Patients who are above or below normal range are also more likely to produce immature eggs during IVF cycles, which then leads to a lower chance of a successful embryo transfer,” Dr. Malik explains. “As a patient’s obesity increases, conception and pregnancy rates decrease as well.”
For patients with an above normal BMI who do conceive, they can have the following pregnancy complications:
- Higher frequency of early pregnancy loss (miscarriage)
- Greater anesthesia and surgical complications if any surgery required
- Greater frequency of hypertension, gestational diabetes, pre-eclampsia, stillbirth, and other pregnancy complications. (Rates of stillbirth are twice as high in obese patients compared to those patients who have a normal BMI.)
- Increased risks of requiring caesarean section delivery. The caesarean section rate is almost 50 percent higher in obese women and the postoperative complications following C-sections are significantly higher.
- Due to larger babies, there is a greater delivery complication rate for those delivering vaginally.
In addition to these complications, we have also seen that obesity can affect outcomes in donor egg treatment. In 2013, SGF’s research department performed a study to see how obesity levels affected birth rates when a woman was the recipient of an egg from a donor. Donor egg treatment traditionally has the highest success rates in our IVF Program, but study results showed that an increase in recipient BMI was associated with a decrease in live birth. Live birth rates were reduced by 21 percent in those recipients with BMI greater than 35 compared to recipients with a lower BMI. There were no significant differences seen in recipients with BMI between 25-30 and 30-35 [4].
It is important to note that reducing BMI through weight loss has been demonstrated to significantly improve fertility treatment outcomes and to lower both treatment and pregnancy complications.
How is male fertility impacted by BMI?
As with women who have fertility complications related to BMI, men suffer from similar complications, since being under or overweight creates a body that is out of balance. When the body is out of balance, normal functions are affected. In men, abnormal semen parameters (i.e. low sperm counts and low sperm motility) have been seen to increase with obesity. “Obese men who are infertile have also been found to have a hormonal imbalance – characterized by decreased levels of testosterone and elevated levels of estrogen – which is an issue that may impair signals from the brain that regulate sperm development,” states Dr. Malik. Obese men are also at risk for impaired spermatogenesis, the process by which sperm are formed, due to increased scrotal temperatures.
Do fertility centers have BMI restrictions for patients who need to undergo treatment?
“At Shady Grove Fertility, we recognize that risks exist at elevated BMIs at or around 35, but that risks increase substantially at a BMI at or above 40 for patients undergoing IVF or a BMI at or above 44 for any patients conceiving through low-tech treatment. Thus, at SGF, patients must have a BMI less than 40 before initiating an IVF cycle and a BMI of less than 44 before initiating IUI cycles,” says Dr. Malik. IVF cycles have a lower weight threshold due to the increased surgical complications that can arise with greater BMI levels.
How can I modify my weight to improve my chances of conception?

If you have been trying to conceive for more than one year, it is recommended that you meet with a fertility specialist. Through a review of your medical history and your diagnostic testing, it can be discerned if weight is the primary factor impacting your fertility or if there are other underlying causes. No matter the diagnosis though, patients are encouraged to maintain a healthy body weight when trying to conceive. We have seen remarkable improvements in treatment success in patients who are able to gain or lose weight, depending on their BMI designation. Balancing diet and limiting exercise was seen to help in underweight patients, and undergoing significant weight loss – which often led to the resumption of ovulation – helped overweight patients.
At SGF, our physicians provide many resources to help patients on their path to parenthood. This help may come in the form of a weight loss program with nutritional counseling, dietary modification, or an exercise program begun prior to treatment. “Our goal is for the patient to be in the best possible overall health before beginning treatment, which will ultimately help the expectant mother have the greatest chance of conception,” Dr. Malik says.
Ideal Weight and Fertility Success
There are many ways in which fertility specialists can help their patients overcome infertility. The majority of these treatment options involve medicinal stimulation, regular monitoring appointments, and for some, surgical procedures. In the case of BMI though, patients and physicians can work together to non-invasively help a woman or man reach an optimal weight for conception. Being aware of the importance of body weight on reproduction can enable couples to maintain their ideal body weight before they begin fertility treatment. When patients have their weight at the ideal level, it can greatly increase their chances of reproductive success and reduce potential risks and complications.
References:





