
Many couples having trouble conceiving are frequently prescribed clomiphene citrate, more commonly referred to as Clomid. Often times, this low-tech treatment option is the first line of therapy for women, especially those who experience irregular or absent menstrual cycles. Prescribed by an OB/GYN or reproductive endocrinologist, Clomid is an affordable oral medication that is used to induce ovulation.
The chance of success with Clomid treatment depends upon a woman’s age and the cause of infertility. In a young woman who does not ovulate regularly, she has a 15–20% chance of conceiving each month on Clomid. Understanding how to optimize each treatment cycle can help couples achieve success with Clomid treatment.
What is Clomid?
Clomid is an anti-estrogen medication that works by blocking the estrogen receptors in the hypothalamus. As a result, follicle-stimulating hormone (FSH) production by the pituitary gland increases, resulting in the development of one or more follicles inside the ovaries. About a week after the last dose of Clomid, ovulation will occur when a surge of luteinizing hormone from the pituitary gland stimulates the developing egg inside the follicle(s) to mature and release.
How much does Clomid cost? Clomid is an affordable medication commonly covered by insurance providers that only costs a few dollars. If insurance isn’t an option when paying out of pocket, Clomid can cost between $25 to $50 per cycle.
Where can a Clomid prescription be filled? Clomid prescribed by your physician can easily be obtained by most local pharmacies, whether they specialize in fertility medications or not.
What are the common side effects? Though it is generally well tolerated, Clomid can lead to cervical mucus changes and thinning of the uterine lining that can negatively impact success rates. As a result, approximately 80% of women taking Clomid will successfully ovulate, but fewer than 50% of patients will conceive. Another risk to consider is the increased chance of multiples – which is around 10% – as compared to the natural rate of twinning, which is between 1-2%.
Tips for Optimizing Fertility Treatment with Clomid
Get a basic infertility work-up
While ovulation is an important part of conception, it isn’t more important than the quality of the male partner’s sperm or the ability for the sperm to access an ovulated egg in the fallopian tubes. For this reason, a full fertility evaluation looking at the sperm quality through a semen analysis and confirming that the tubes are open with an HSG, should be completed prior to starting any treatment, including Clomid. Why spend time on a treatment that may not work due to other unforeseen factors?
Add Monitoring to the Cycle
While the American Congress of Obstetricians and Gynecologists’ guidelines for Clomid treatment do not require monitoring during a Clomid cycle, valuable time-saving information can be gained by adding an ultrasound and hormone monitoring after the last dose of medication.
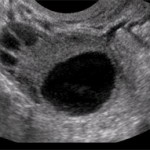
Monitoring appointments consist of an ultrasound and bloodwork. The ultrasound, completed intravaginally, allows the physician to visualize the thickness of the uterine lining and the ovaries, more specifically the number of follicles within them. The bloodwork shows the trend of pre to post-stimulation hormone levels; increased levels of estrogen indicate follicular development.
These two measures of the progress of the cycles tells physicians about three important events during stimulation.
1. Did it work? This seems like a no-brainer, but the first thing a physician learns from monitoring the progress of the cycle is if a follicle was recruited and developed. Finding the correct dosage that results in the development of a single follicle in the beginning is a bit of guess and check. Some women will respond to a 25 mg dose, while others can require up to 150 mg before follicular development starts to occur. Starting with a conservative dose until the physician knows how a patient will respond is the best approach, as overstimulation can result in the development of more than one follicle and, as a result, an increased risk of multiples. In an unmonitored cycle, the physician would base the response to medication solely on if the cycle resulted in a pregnancy and then adjust the dosage accordingly.
So what if it doesn’t work? Lack of response indicates to the physician a higher dosage of medication is needed. This higher dose can start the same day since the patient is still in the follicular phase of her cycle. The ability to know that the dosage was ineffective early in the treatment cycle saves the patient nearly an entire month.
2. Is the lining thick enough for implantation? The second factor that monitoring can tell a physician is how the lining responded to the Clomid. Some patients using Clomid will suffer from a thinning of the uterine lining, making for a less than optimal environment for embryo implantation. Should this occur, physicians can help to supplement the thickening of the lining with an estrogen suppository. In some cases a follicle will develop, but pregnancy may not have occurred because the lining was too thin – a factor that the physician wouldn’t be aware of without a monitoring cycle.
3. Was there an over-response to medication? Unmonitored cycles can result in an increased chance of multiples, which is risky for both mother and babies. Multiples can occur when several follicles are developed and ovulated in a single cycle. Monitoring can tell the physician when an unsafe number of follicles have been developed, allowing them to advise the patient to abstain from intercourse to avoid the increased risk of a higher order pregnancy.
Add a Trigger Shot
While under the care of a reproductive endocrinologist, the stimulation phase of a Clomid cycle in most cases ends with a trigger shot. The trigger shot provides the final maturation signal to the developing follicle and sets ovulation in motion. One of the biggest benefits to a trigger shot is the increased ability to correctly time intercourse at home or insemination in the office. The majority of patients will be instructed to administer their trigger injection between 6 and 10 p.m. Two days later, the IUI – if that is your planned method of insemination – will be scheduled at one of our 18 full service locations. Intercourse on the night of the trigger shot is encouraged so that sperm is present in the reproductive track at the time of ovulation. Those patients using timed intercourse will be instructed to also have intercourse the day of the trigger shot and then again two days later.
Consider an Intrauterine Insemination
Clomid treatment helps with the first part of the equation, developing an egg and inducing ovulation. The other part of the equation centers around getting the egg and sperm to meet. With Clomid treatment, there are two common methods used to facilitate this introduction, with the most familiar to patients being timed intercourse. Some couples, especially those still at their OB/GYN, will start with this option, using ovulation predictor kits to help determine the right time for intercourse.
The second option is an intrauterine insemination (IUI), which is usually done while under the care of a fertility doctor. During an IUI, a concentrated specimen of sperm is placed in the uterus. The procedure is completed in the office and does not require sedation. An IUI may be needed if conception has not occurred due to mild sperm abnormalities or for unexplained reasons.
Use a Fertility-Friendly Lubricant
Another side effect associated with Clomid is vaginal dryness that can make intercourse uncomfortable. Choosing a fertility-friendly lubricant such as pre-seed can help alleviate dryness and not negatively impact sperm. It is not, however, suggested to use many of the other over the counter personal lubricants as they can have a negative effect on the sperm.
Talk to your Provider about trying Femara
Femara (generic name Letrozole) is another oral medication that can be used to induce follicular development. Femara works by suppressing estrogen levels, causing the brain and pituitary gland to increase the output of follicle-stimulating hormone (FSH). The chances of pregnancy with Femara have been found to be the same as with Clomid, between 15-20% depending on diagnosis and the female partner’s age.
One of the major benefits of using Femara is the decrease of detrimental side effects, such as thinning of the endometrial lining and the risk of multiples. Femara supports more unifollicular development, allowing a single follicle to emerge as the dominate follicle that is ultimately ovulated. Since often times only one follicle develops, the chance of multiples is lower. While Femara is relatively new in the fertility realm, it has been shown to be helpful for women with ovulatory disorders like polycystic ovary syndrome (PCOS).
For women beginning fertility treatment, it’s important for them to know that Shady Grove Fertility uses a stepped approach to care, starting with the least invasive treatment options to start. Fifty percent of treatment programs at SGF are low-tech options such as timed intercourse or IUI, giving patients the same chance of conception that the fertile population has on a monthly basis (15-20%).
If you have questions regarding infertility treatment or would like to schedule a new patient appointment, please call our New Patient Center at 877-971-7755 or click to schedule an appointment.





