Medical contribution by Jason G. Bromer, M.D.
Jason G. Bromer, M.D., is board certified in obstetrics and gynecology and reproductive endocrinology and infertility. He has been involved in cutting-edge research in fertility preservation for cancer patients, pregnancy implantation, and methods of embryo selection for in vitro fertilization.
When beginning the infertility treatment process, diagnostic testing will be the first step you take before your clinical plan can be created. Infertility is diagnosed based on the results of three main tests: day 3 hormone bloodwork and a hysterosalpingogram (HSG) for the female partner, and a semen analysis for the male partner. Each test looks at a different component significant to conception:
- Day 3 hormone bloodwork: FSH (Follicle-Stimulating Hormone) and AMH (Anti-Müllerian Hormone) provide insight about egg quantity, while estrogen and LH (Luteinizing Hormone) levels can indicate information about the maturation of follicles.
- Hysterosalpingogram (HSG): Determines the condition of the fallopian tubes and uterus.
- Semen analysis: Evaluates the quantity and quality of the male partner’s sperm, specifically looking at parameters such as sperm count, morphology (size and shape), and motility (the number moving in a forward progression).

Prior to starting diagnostic testing, many patients have already had their blood drawn and know what to expect regarding hormone evaluation. Most patients, though, have not experienced a hysterosalpingogram (HSG).
Fear of the unknown can make many patients nervous or apprehensive about this aspect of their diagnostic work-up. However, learning all that SGF does to make the test more manageable is hopefully reassuring.
Why do I need a hysterosalpingogram (HSG)?
After ovulation, a current in the body pushes the egg into the fallopian tubes where the sperm and egg will meet and fertilization can occur. Once an egg is fertilized, an embryo will develop and continue through the fallopian tubes until it reaches the uterus, where it will implant into the uterine lining. The hysterosalpingogram is performed routinely for patients having difficulty conceiving because it is an excellent test that not only can confirm that a woman’s fallopian tubes are open, but can also assess whether the uterus has a normal shape. It can also make sure the cavity is not affected by fibroids, polyps or scar tissue.
The HSG procedure
Prior to starting the HSG, the patient must produce a urine sample. This is an important step as it allows the practitioner to be sure that the patient is not unknowingly pregnant prior to starting the HSG. Should a patient be pregnant, the contrast used to fill the uterus can harm or displace the growing fetus, resulting in an increased risk of miscarriage.
At the start of the procedure, a speculum is inserted into the vagina in order to view the cervix, similar to a Pap smear. The cervix is cleaned with an antiseptic solution; then, a thin, plastic catheter, generally about the size of the tip of a pen, is placed inside the cervix. Once placed, a small amount of contrast, usually two to three teaspoons, is passed through the catheter into the cervix, filling the uterus and fallopian tubes. Contrast is used, as opposed to dye, which is a colored substance that cannot be seen on an x-ray, whereas contrast can.
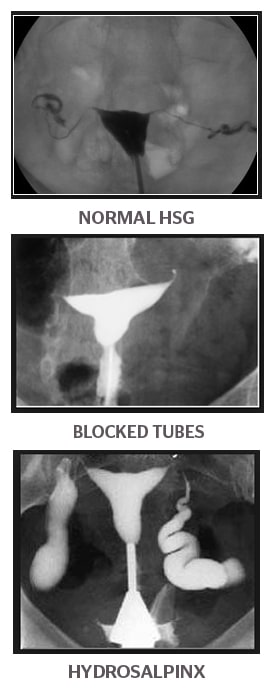
While lying flat on the table, a special type of X-ray imaging technology called fluoroscopy is used to provide a “live” X-ray that allows the practitioner to watch as the contrast fills the uterus and travels into the tubes. The tubes are considered open when the contrast is able to move completely through the length of the tube, spilling the contrast out on the other side. This indicates that the tubes are open and available to “pick up” an egg post-ovulation. Immediately following the HSG test, patients will receive preliminary results from their practitioner. The images taken throughout the procedure are then sent to the ordering physician, along with the practitioner’s findings.
Side effects and risks
There are several fairly common side effects associated with HSG tests: abdominal pain and/or discomfort, feeling crampy or achy, and vaginal spotting and/or watery discharge. When spotting or discharge occurs, we encourage patients to use sanitary napkins or pads as opposed to tampons. We also encourage our patients to speak with their physician about taking some over-the-counter pain reliever following the test to reducing any cramps or discomfort.
While uncommon, a risk associated with HSG is infection. Patients that have a diagnosed or suspected problem with their fallopian tubes – such as a history of ectopic pregnancies or a hydrosalpinx – will likely be prescribed an antibiotic to be taken in advance. An HSG will not bring on menses, so if you experience a full menstrual flow, develop a fever, or continue to feel pain for more than a few days, you should speak with your physician. If it is after hours, you should call Shady Grove Fertility’s answering service.
Why choose SGF for your HSG?
Shady Grove Fertility places high value on patient safety and comfort and goes out of our way to minimize discomfort. Here’s how:
We encourage taking a pain reliever 30 to 60 minutes prior. Many women feel some cramping for about 2 minutes when the contrast is filling the uterus. Therefore, we strongly encourage taking an over-the-counter pain reliever (such as ibuprofen) 30 to 60 minutes before the test to reduce feelings of pain or discomfort. This will help tremendously.
Also, speak with your doctor about taking pain medicine 30 to 60 minutes before the procedure especially if you have a history of ectopic pregnancies or a hydrosalpinx.
We have very experienced clinicians who perform HSGs. The clinicians at our practice who perform HSGs perform thousands each year and have the experience and expertise to help make your experience as comfortable as possible.
We encourage communication. We encourage you, if you are feeling any discomfort during the test, to communicate with your clinician performing the test, let us know if it hurts, and we may be able to make some adjustments to make you more comfortable.
We are selective about contrast and instrument type. We select a contrast that is known to cause the least amount of cramping and an instrument that is known to cause the least amount of discomfort.
We care about your comfort. We perform this procedure on a GYN table, which makes patients more comfortable, compared with a hospital table common in other locations.
We don’t tell our patients the procedure will be 100% painless but we reassure that we will do everything in our power to make the test more comfortable.
Here’s what our patients are saying:
- “After reading all that horror stories on internet, I was so nervous! It was nothing at all. Like a regular OB exam, but a little bit longer.” – Tanya
- “I had my HSG done a few months ago and I did have some pretty intense cramping during mine. I have endometriosis, so I’m used to intense cramps, but I was pretty uncomfortable through the procedure, but it was quick, and it wasn’t anything that I couldn’t bare.” – Stacy
- “It was not at all painfully except for 2-4 seconds of our very known menstrual pain which occurred when they filled with the contrast dye.” – Ranuak
- “My HSG went very smoothly. I only felt a little pinch when they inserted and inflated the catheter. When they injected the dye it just felt like a very dull menstrual cramp and then it was over before I knew it!” – Jennifer
Common patient questions about HSGs
How long does an HSG take? While the actual procedure takes about 5 minutes, you should plan to arrive for your HSG 30 minutes prior to your scheduled appointment. You can also expect to be with us for 30-45 minutes after the scheduled HSG start time.
Is it okay to drive home by myself after the test? The standard operating procedure for an HSG does not call for sedation. You are unlikely to have pain following the procedure, but you may feel crampy or achy. The majority of our patients are able to drive after an HSG and even immediately return to work.
When is the best time during my cycle to schedule the HSG? The test should be scheduled after your period ends, but before you expect to ovulate – usually between days 5 to 12 of your menstrual cycle. To figure out the days of your cycle, count day 1 as the day your period begins.
Where can HSGs be performed? HSGs can be completed in many healthcare environments, including hospitals, radiology labs, or other free-standing centers. Shady Grove Fertility has two free-standing HSG suites located in Rockville, MD and Towson, MD.
Do I have to complete my HSG at a Shady Grove Fertility facility? No, Shady Grove Fertility physicians routinely make diagnostic and treatment decisions based on HSGs performed at facilities other than our own. Occasionally, however, the information on an HSG done at an outside facility may be inconclusive or not provide all of the information needed for the best medical recommendation. In these situations, your Shady Grove Fertility physician may recommend repeating the HSG to obtain necessary information.
Because we take great pride in the lengths to which we are able to go to make sure women are as comfortable as possible during an HSG, many physicians refer their patients to SGF for an HSG.
Who can administer an HSG? HSGs can be performed by infertility specialists, obstetrician-gynecologists, radiologists, physician assistants and other health care providers. Health care providers performing HSGs should be trained in performing pelvic exams and be technically proficient with the HSG technique. They should also be able to evaluate its findings and report them comprehensively.
Will I have insurance coverage for my HSG? Most – but not all – insurance policies will cover the expense of an HSG completed at Shady Grove Fertility. The choice to have the HSG performed at Shady Grove Fertility versus another facility is ultimately up to you. Patients whose insurance policy does not extend HSG benefits at Shady Grove Fertility will incur a charge for the procedure and will be responsible for its payment. The cost versus the benefits can be discussed with your primary Shady Grove Fertility physician, as well as other questions you may have about the HSG.
How soon after the HSG can I resume intercourse? Generally, we want patients to abstain from intercourse until after vaginal spotting or discharge stops, usually 1 to 2 days after the HSG.
So much of the infertility treatment process is about narrowing down the cause(s) of an individual’s infertility. The HSG, though not commonly known, is a beneficial way that your physician can determine the best path to help you on your journey to reproductive success.
To schedule a virtual consultation with an SGF physician, please call our New Patient Center at 1-888-761-1967 or submit this brief form.
Editor’s Note: This post was originally published in August 2014 and has been updated for accuracy and comprehensiveness as of December 2020.