Medical contribution by: Stephen J. Greenhouse, M.D.
When choosing a fertility center, it’s important to research the many different options available to you. Finding a center relatively close to your home; a center that values patient care; and a center that has reproductive endocrinologists with extensive experience, are all very important components of the decision-making process. But the most important factor to research often comes down to the center’s infertility success rates. By learning a few simple points, you’ll be able to determine what infertility success rates really mean, without needing an advanced degree in statistics.
Reporting Infertility Success Rates
In 1992, Congress passed the Fertility Clinic Success Rate and Certificate Act—endorsed by the American Society for Reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technology (SART)—which requires clinics to collect and make public the results of assisted reproductive technology (ART) treatments including in vitro fertilization (IVF), frozen embryo transfer (FET), and donor egg treatment. On SART’s website, you can view infertility success rates for individual fertility centers and also view the national data summary, which depicts the national average, based upon data from every fertility center in the country.
Learn the Appropriate Lingo
Before viewing infertility success rate data, it’s helpful to learn the terminology associated with reporting assisted reproductive technology.
Initiated cycle: An initiated cycle refers to the start of medications with the intent to proceed with in vitro fertilization (IVF) treatment.
- Example: The center had 4,900 initiated cycles in 2013.
- Explanation: As patients can go through multiple cycle attempts within 1 year, it’s worth remembering that the number here does not mean 4,900 individual patients. It is merely the amount of IVF cycles that a center initiated and may or may not have continued forward.
Cancellation: Unfortunately, some cycles will have to be cancelled before an egg retrieval can occur. This is usually due to a poor response to medication. It’s in the best interest of the patient to cancel the cycle rather than continue to egg retrieval if a positive outcome is unlikely. Age can also be a factor that affects how well a woman’s body responds to the medicinal stimulation.

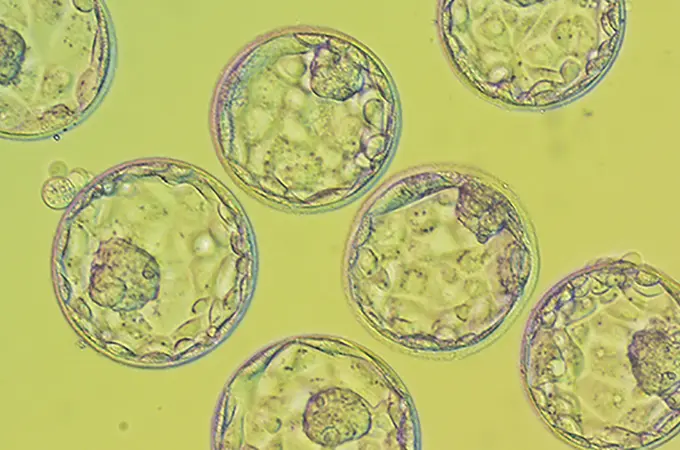
Retrieval: An egg retrieval is the actual attempt to obtain eggs from the ovarian follicles. In order to get to the stage of embryo transfer (in which a physician places a fertilized embryo into the woman’s uterus), a successful retrieval must occur.
- Example: The center had 4,900 initiated cycles, but only performed 4,400 egg retrievals.
- Explanation: The missing egg retrievals are due to cycle cancellation.
Transfer: An embryo transfer is the placement of one or more embryos back into the uterus. Transfer can only occur after fertilization between the retrieved eggs and sperm has taken place in the lab and the embryo is given 5 days to develop, ideally into a blastocyst.
- Example: The center performed 4,400 egg retrievals but only performed 3,900 embryo transfers.
- Explanation: Why is there a discrepancy here? Unfortunately, some embryos do not develop to the point of transfer. The physician and embryologist want the highest quality embryos for transfer, and if they’re not developing properly in the lab, they are unlikely to properly develop in utero. Another reason a transfer may not occur is due to genetic testing. Genetic testing affords couples the ability to ensure that they do not pass certain diseases and disorders onto their offspring. Thus, sometimes genetic testing reveals that an embryo is abnormal, and therefore the physician would not schedule a transfer. Finally, egg and embryo freezing would also mean that a transfer would not take place. Women who electively freeze their eggs may return one day, but for now the intention is to preserve their eggs for the future, not for immediate transfer. For other women, the physician may perform a freeze-all cycle, in which the patient elects to freeze all of the embryos, rather than transfer. Among other reasons, this most commonly occurs if a woman’s progesterone levels are too high leading up to transfer, which has been shown to increase the potential for miscarriage. By freezing the embryos and then waiting to transfer when progesterone levels have returned to a normal level, women are afforded the best possible chance to conceive.
- Extending Your Fertility Treatment: Frozen Embryo Transfers (FETs)

Clinical pregnancy: A clinical pregnancy refers to the identification of a pregnancy sac in the uterus—not just a positive pregnancy test.
- Example: Out of 3,900 embryo transfers, the center had 1,800 clinical pregnancies in 2013.
- Explanation: That seems like a very significant drop, and probably rather alarming to patients new to fertility treatment. It’s important to think about the natural rate of fertility each month: women under the age of 35—who are trying to conceive on their own—only have a 15 percent chance of conceiving each month, which declines each month after 4 to 5 months of trying. After trying for 2 years, the chance of conception each month drops to approximately 1 percent. Not every egg will become a pregnancy, and that statistic holds true for fertility treatment as well. While the physicians and embryologists do everything in their power to help patients build their families, there is an element of ‘nature’ at play here, not just science. It’s important to also remember the 15 percent chance of naturally conceiving each month when you view success rates. Even the best centers only show success rates that range from 40 to 60 percent. So while at first glance, that may not seem very high, it really is impressive when you think about the natural rate of conception being only 15 percent in any given month.
- Understanding Infertility Success Rates Infographic
Miscarriage: Unfortunately, miscarriages are common for both women going through fertility treatment and women who conceive without assistance. In fact, it is estimated that 1 in 4 pregnancies result in a miscarriage, sometimes even before the woman realizes she is pregnant. Given the occurrence of miscarriages, it’s important to look at a fertility center’s ongoing pregnancy/live birth delivery rate.

Ongoing pregnancy/live birth rate: The ongoing pregnancy/live birth rate represents the number of patients who have delivered a baby or are still pregnant. This number will always be lower than the clinical pregnancy rate due to the possibility of miscarriage. The ongoing pregnancy/live birth delivery rate is the most important number to Shady Grove Fertility, as we define success in the same way you do—taking home a baby.
How do fertility centers calculate infertility success rates?
Success rates can vary for many reasons. The age of the female partner (as mentioned earlier) is the most important factor when women are using their own eggs. As women age, success rates decline, particularly over the age of 35. This decline is partially due to a woman’s reduced chance of getting pregnant through ART (and without ART) as she gets older, but it is also due to the higher risk of miscarriage associated with increasing age, especially over 40. Evidence of age’s effect on pregnancy rates is undeniable, especially when viewing donor egg treatment success rates: the eggs that a donor recipient uses are from a woman who donated her eggs in her 20s to early 30s, leading to much higher success rates.
Success rates can also vary based on the number of embryos transferred. Transferring more embryos at one time does not increase the chance of live birth significantly, but it can increase the risk of a multiple pregnancy. At Shady Grove Fertility, we advocate for single embryo transfer (eSET) in good prognosis patients, because the risks associated with multiple pregnancy (twins, triplets, etc.) are too great on the health of the mother and the babies. The ideal fertility center maintains high success rates while transferring the fewest amount of embryos. At Shady Grove Fertility, we have been successful at reducing multiple pregnancies over time, due to our practice of eSET.
As SART says on their website, “It is important to note that patient characteristics vary among programs; therefore, success rates should not be used to compare treatment centers.” Additionally, success rates are important, but they can vary greatly between individuals, with many patients requiring several treatment cycles to have a baby.
When researching a center, it is important for one to evaluate a combination of outcomes—delivery/live birth rate per initiated cycle, implantation rate, rate of multiples, and the average number of embryos transferred. The time it can take to become pregnant is a major concern for couples who are struggling with infertility. Thus, it’s important to view a center’s ongoing pregnancy/live birth rate in comparison to the initiated cycle rate. If a center has a high ongoing pregnancy/live birth rate, it’s an important indicator of how effectively a center can help you to conceive. Before deciding on a treatment center, we recommend that you schedule a consult with a physician so that he/she can help you interpret the success rates as they apply to your medical profile and history.