
The nature of infertility care has changed dramatically in the last 30 years, as technology has paved the way for patients to have the best chances of conception. This revolution in care has particularly affected the embryo transfer stage of in vitro fertilization (IVF). When a woman undergoes IVF, her eggs are retrieved and then fertilized with her partner’s (or donor’s) sperm. Once the fertilized embryos have matured into high-quality embryos (usually on the fifth day after fertilization), it is time to decide how many embryos should be transferred. This is where Newsweek’s article “Twins: The Fetal Paradox” comes into play.
In the early days of IVF, fertility specialists would often recommend transferring multiple embryos. “People were hedging their bets,” said Dr. Robert Stillman, medical director emeritus at Shady Grove Fertility, who was interviewed for this piece. The technology was not strong enough in the past, so transferring multiple embryos provided a patient with the best possible chance to have at least one healthy embryo develop. In the modern era though, laboratory conditions have developed extensively, enabling embryologists to accurately assess the highest quality embryos to transfer. In good prognosis patients (see below), transferring a single embryo (known as elective single embryo transfer or eSET) will yield the same results as transferring multiples – but without the risks associated with a multiple pregnancy. SGF has been a long-term advocate of eSET and the number of patients who select eSET at our practice is nearly five times higher than the national rate.
eSET Frequently Asked Questions
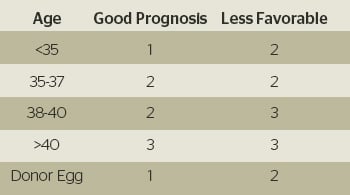
What characterizes a good prognosis patient during IVF treatment?
Women who statistically have the best possible chance of success with treatment are considered good prognosis patients. Factors that determine a good prognosis are the following: the American Society for Reproductive Medicine (ASRM) age guidelines (see below); women without a history of failed IVF treatment; and/or the availability of high-quality blastocyst-stage embryos.
What health risks are associated with multiple pregnancies?
While plenty of healthy twins and triplets are born every day, multiple pregnancies can present additional risks for both the mother and her babies. There is an increased chance of miscarriage, bleeding, extended periods of bed rest, gestational diabetes, pregnancy-induced hypertension, and the need for cesarean sections. The babies can have low birth weights, sometimes with one twin growing at the expense of the other. They are more likely to be delivered prematurely, need intensive care after birth, suffer from developmental disabilities, and even have increased mortality rates. Due to these risks, we encourage our good prognosis patients to select eSET, ultimately reducing the possibility of a multiple pregnancy.
What are my chances of pregnancy if I only transfer a single embryo?
Whether transferring one or two high-quality blastocyst-stage embryos, patients with a good prognosis can expect the same conception rates. As a result, in 2013, nearly 80 percent of all pregnant patients in the SGF IVF Program had a singleton pregnancy. Additionally, 66 percent of patients under the age of 38 participated in the eSET program.
If eSET is the safer choice and has equivalent success rates, why do some patients still transfer multiple embryos?
At SGF, we often talk about how we provide patients with individualized care. This is important for a very obvious reason: no two patients are alike. Each patient’s history of trying to conceive and their individual diagnosis helps physicians recommend the best course of treatment. While our physicians ideally like to transfer high-quality blastocyst-stage embryos, this isn’t always possible for every patient. Thus, in incidences where embryo quality is a bit less than hoped for, the physician will determine if transferring multiple embryos would be beneficial. For those patients who have had earlier unsuccessful cycles with a single embryo, the physician also may recommend transferring an additional embryo.
The decision ultimately lies with the patient when it comes to eSET or transferring multiple embryos. But our physicians will always encourage eSET for those patients who have a good prognosis.
Insurance Companies Begin to Encourage eSET
One of the largest motivators for patients who want to transfer multiple embryos is the cost associated with fertility treatment. Many insurance companies do not cover the cost of treatment at all, or some will cover one cycle, but not additional ones. This is a concern for some patients, who think that transferring multiple embryos provides them with a better chance of conception in one cycle versus having to possibly perform multiple cycles. Due to the risks involved with multiple pregnancies, we do not encourage transferring multiple embryos in good prognosis patients, but we are conscious of the financial investment of treatment and have many financial programs to help our patients on their path to parenthood.
Some insurance companies are also starting to change their practices – if patients choose eSET and the first IVF cycle fails, the insurance company will cover the cost of the second transfer. “We’re hoping that this will be the wave of the future,” Dr. Stillman said. “It’s in insurance companies’ best interest: IVF costs are minimal. Premature twins or triplets can present lifelong complications and costs.”
Read the complete article to learn more about elective single embryo transfer.
If you have questions regarding infertility treatment or would like to schedule a new patient appointment, please call our New Patient Center at 877-971-7755 or click to schedule an appointment.



