For patients experiencing recurrent early pregnant loss or repeated failed implantations, there is often a common misbelief that the maternal immune system is killing the embryo when it is trying to implant and the root cause of this is due to what are called natural killer cells (aka NK cells).
There are two types of NK cells and they both have important – and distinct – roles in the fertility journey. Let’s break down the facts versus fiction when it comes to NK cells.
What are NK cells?
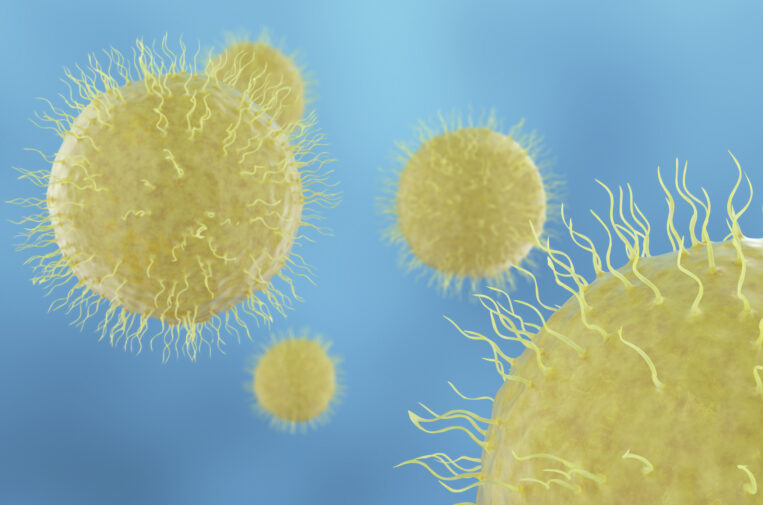
NK cells can be found in two areas: in the uterus, called uterine NK cells, and additionally in the blood stream, called peripheral NK cells.
Peripheral NK cells
The cells in the blood are the ones that earned the name – they are indeed “killers” as they fight off cancer cells and cells that have been infected by viruses.
Uterine NK cells
Uterine NK cells are quite different. They do not fight off viruses and cancer cells. Uterine NK cells have different receptors along their wall that make them completely distinct from the peripheral NK cells found in the blood. This means when you have your blood drawn to test for NK cells, this is testing for peripheral NK cells and not uterine NK cells.
What are uterine NK cells’ function?
Fact: Research shows that uterine NK cells do not kill embryos.
Uterine NK cells are actually very important to remodeling and shaping the spiral arteries, which bring blood supply to the developing embryo, and thus have an important role in building a healthy placenta.
“I live in Florida, so let’s use this easy analogy: when the ocean hits the sand, it starts to recede,” shares Rachel Sprague, M.D., who cares for patients in SGF’s St. Petersburg, FL location. “So, if you want to make a little tidal pool on the beach, you’ll need to make a canal through the sand that connects the ocean to the tidal pool – and you need to make the canal narrow enough for the ocean water pressure to push through and make the canal deep enough so it the water does not just pull back into the ocean. If you do not make that canal just right, it will not bring the water correctly from the ocean to your tidal pool. This is how I describe the uterine NK cells – they help carve the path for exchange of oxygen and nutrients from the uterus to baby.”
Do uterine NK cells cause recurrent early pregnancy loss?
The concern around recurrent early pregnancy loss and repeated failed implantation is that the uterine NK cells are actually malfunctioning rather than over-functioning. By malfunctioning, they are not doing a good job at remodeling the blood flow (i.e. building the canal through the sand), leading to poor development of the placenta and putting the pregnancy at risk.
“Does the maternal immune system have a role in pregnancy and implantation?” asks Dr. Sprague “Yes. But is the answer destroying these uterine NK cells? It is more complex than that. And we see that when we look at immunosuppressive options that block the maternal immune system — they do not work as well as we would hope.”
Such therapies such as corticosteroids, IVIG, Granulocyte-colony stimulating factor, intralipids, intrauterine hCG, and low dose naltrexone are some of those medications that have been given routinely to patients in an aim to block the maternal immune system. However, these therapies lack any robust evidence that they are truly helpful, and on top of that, many studies also show that these therapies can have the reverse effect, leading to increased pregnancy loss. More importantly, as the studies are small, we lack import safety information for mother and baby.
What is the solution?
We are still learning more about how to modulate these cells – meaning, we are trying to teach them how to work better rather than to block their actions. But we still need more time, effective studies, and safety information before we truly know how to do this.
In the meantime, there are very good studies that support the idea that success is in the hands of the embryo.
“Each embryo, just like each person, is very different,” shares Dr. Sprague. “And when we continue to transfer healthy embryos, success goes up and up and up. Thus, find the right embryo and this leads to our end goal of the right baby for you.”
Medical contribution by Rachel Sprague, M.D.
Rachel Sprague, M.D., earned her medical degree from the University of Florida College of Medicine. It was during this time that her interest in reproductive medicine came to light when she was exposed to the concept of in vitro fertilization and the intricacies of early pregnancy. The interest intensified throughout her clinical rotations where she experienced first-hand the bond between patients and their physicians.