Medical contribution by Stephanie Beall, M.D., Ph.D.

Many people have heard of in vitro fertilization (IVF), a commonly used fertility treatment. Some people erroneously assume that IVF is the only form of fertility treatment, without realizing that most patients do not begin their treatment journey with this approach. Most patients actually start with a low-tech treatment option, such as timed intercourse or intrauterine insemination (IUI). Regardless of where you start your journey, if it involves IVF, let the information in this fact sheet be your guide.
What is IVF?
In the simplest terms, IVF is a procedure in which a physician will remove one or more eggs from the ovaries that are then fertilized by sperm inside the embryology lab. IVF is the most successful treatment a couple can do using their own eggs and sperm (or donor sperm). IVF has become mainstream, widely accepted, and continues to grow, due to significant technological advances.
Who Needs IVF?
There are many types of diagnoses that may lead to patients undergoing IVF. Here are some of the most common indications for IVF treatment:
- Fallopian tube damage/tubal factor: In order to treat significant tubal damage, surgical repair or IVF (which bypasses the fallopian tubes) are the available treatment options. Your physician and your individual medical history can help determine the best course of action for your diagnosis.
- Male factor infertility: In nearly 40 percent of infertility cases, the diagnosis is male factor infertility. The cause of male factor is often unknown, but some problems have been identified, including sperm production disorders, abnormalities of the reproductive tract, difficulty with erections or ejaculation, endocrine and immune disorders. Intracytoplasmic sperm injection (ICSI) has made significant strides for patients with male factor infertility. Learn more below.
- Endometriosis: Endometriosis may be effectively treated with either surgery or IVF depending on the severity of endometriosis and other factors that could impact the chance of pregnancy.
- Age-related infertility: As a woman ages, her ovarian reserve (egg supply) will decrease, with egg quality also negatively impacted. In many cases, this reduced ovarian function can be overcome through the use of IVF.
- Unexplained infertility: Approximately 10 percent of couples will have no identifiable cause of infertility after completing a comprehensive evaluation. IVF is often successful, even if more conservative low-tech treatments have previously failed.

Genetic abnormalities: For patients who are at risk for passing to their children a genetic disorder, preimplantation genetic diagnosis (PGD)—in which a few cells are removed from an embryo and tested for genetic disorders—can provide information about which embryo(s) the physician should transfer back to the female partner. IVF has created the ability to perform PGD, as fertilization of the embryos occurs in the lab. Additionally, for patients who experience recurrent pregnancy loss or have repeated unsuccessful IVF cycles, preconception genetic screening (PGS) provides the opportunity to discover if the underlying cause may exist on the genetic level.
What is the Timeline for an Average IVF Cycle?
In a normal ovulation cycle, one egg matures per month. The goal of an IVF cycle is to have many mature eggs available, as this will increase the chances of success with treatment. In order for there to be more than one egg available, stimulation of the ovaries needs to occur.
Part I: Stimulation of the Ovaries
In the stimulation phase of an IVF cycle, a patient will use injectible medications for approximately 8 to 14 days to stimulate the ovaries to produce eggs. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH), both produced naturally within the body, comprise the medications. During the stimulation phase, patients will come into the office roughly 7 to 8 times for morning monitoring. Monitoring allows the physician to track the progress of the cycle and adjust medication dosages as needed. During a monitoring appointment, the patient will undergo an ultrasound and bloodwork:
- The transvaginal ultrasound measures the growth of the egg-containing follicles and the thickness of the uterine lining, both of which should be increasing throughout the stimulation phase.
- A nurse or clinical assistant will draw blood at each appointment to measure estrogen and progesterone levels. This level is another indicator of the growth and maturation of the eggs, and it rises as the follicles grow.
On the afternoon of a monitoring appointment, the patient can expect a phone call from her nurse with updates, including any changes in medication dosing and to coordinate the next monitoring appointment.
The Trigger Shot
The trigger shot is the final step in the stimulation phase of treatment. Depending on the patient’s individual protocol, she will either have a human chorionic gonadotropin (hCG) or Lupron trigger shot. This shot helps the developing eggs to complete the maturation process and sets ovulation in motion. Timing is very important here, as the physician must perform the egg retrieval prior to the expected time of ovulation.
Part II: Egg Retrieval
A physician will perform your egg retrieval procedure at one of Shady Grove Fertility’s ambulatory surgery centers (ASC) in Rockville, MD, Towson, MD, or Chesterbrook, PA. On the morning of your egg retrieval, a physician will meet with you before the procedure to review your protocol. You will also meet with an anesthetist, who will review your medical history and will administer the IV fluid you will receive prior to the start of the procedure to induce sleep.
- Obtaining the sperm: If patients are using a fresh sperm sample, a lab technician will come to accept the sample. If you are using a frozen sperm sample or donor sperm collected at a previous date, the technician will verify those details with you. Our andrology lab will clean and prepare the sperm, so that the healthiest sperm are brought together with the eggs for fertilization (after the physician performs the egg retrieval).
- Obtaining the eggs: The egg retrieval itself takes about 20 to 30 minutes. During the procedure, the physician will guide a needle into each ovary to remove the egg-containing fluid in each follicle. The physician utilizes an ultrasound during the procedure to see where to guide the needle. Recovery will take about 30 minutes and patients are able to walk out on their own, though someone will need to drive them home since they had been under anesthesia.
- What to Expect the Day of Your Egg Retrieval (Video)
Part III: Fertilization
After the egg retrieval, the embryologist will sort and prepare the eggs and sperm. There are two ways that fertilization can take place: conventional insemination or ICSI. The physician and patient will discuss which method to use based on sperm quality; this is traditionally planned in advance. In some cases, the embryologist may see that semen parameters for conventional insemination are not being met, so she/he will recommend the switch to ICSI to produce the greatest chance of success. Your clinical team will let you know if they recommend an unanticipated ICSI procedure.
- Conventional insemination: For conventional insemination, the embryologist takes the prepared sperm sample and isolates the healthiest sperm. He/she will then incubate this sperm with the eggs in a Petri dish. This gives the egg and sperm the opportunity to find one another and fertilize.
Part IV: Embryo Development
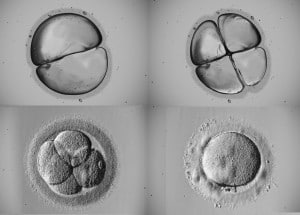
Embryo development begins after fertilization. An embryologist examines each developing embryo every morning for the following 5 to 6 days. The goal is to see progressive development, with a four-cell embryo on day 2 and an eight-cell embryo on day 3. After the eight-cell stage, rapid cell division continues and the embryo enters into what is called the blastocyst stage at day 5 or 6. It is your physician’s goal to transfer the highest-quality embryo or embryos to give patients the greatest chance of reproductive success.
Part V: Embryo Transfer
The embryo transfer is a simple procedure that only takes about 5 minutes to complete. There is no anesthesia or recovery time needed. When your nurse schedules your transfer, she will notify you and provide instructions on when to arrive and how to prepare. You need to have a full bladder for the procedure. It’s important to drink the specific amount of liquid recommended 30 to 40 minutes ahead of time.
You will review your cycle with the physician and the number of embryos recommended for transfer. The embryologist will load the transfer catheter in the embryology lab with the embryo; upon entering the patient’s room, the embryologist will again confirm the patient’s last name and the number of embryos in the catheter. The physician will insert the catheter into the uterus and push the embryo through with a small amount of fluid. An external abdominal ultrasound provides visual guidance to the physician throughout the procedure via a monitor.
Once the physician transfers the embryo, he/she will slowly remove the catheter. Since the embryo is invisible to the naked eye, the embryologist will then examine the catheter under a microscope in the lab to ensure that the embryo was released. The nurse will give you instructions for the following two weeks until it’s time for the beta pregnancy test.
Part VI: The Beta Pregnancy Test
Two weeks after the embryo transfer, a nurse or clinical assistant will perform a blood pregnancy test. This test is frequently called a “beta” because it measures the beta chain portion of the hCG hormone emitted by the developing embryo.

Though many patients are tempted to take an at-home pregnancy test, we caution against it, as these tests can render false positives or negatives. There is nothing inherently wrong with at-home pregnancy tests, but in the instance of IVF, the blood test is more accurate and reliable. Earlier, we spoke about the trigger shot, which can either be Lupron or hCG. If you have an hCG trigger shot, it may remain in the blood and show up on an at-home pregnancy test, possibly rendering a false positive. The urine test cannot discern the difference between the hCG in the trigger shot or the hCG seen elevated during a pregnancy. It’s better to wait the two weeks (though we definitely know how hard it is) and have the beta pregnancy test.
Affording IVF Treatment with the Shared Risk 100% Refund Guarantee Program
Our Shared Risk 100% Refund Guarantee Program financially insures you against the risk of not being successful. In this program, you elect to pay a flat fee that covers up to six cycles of IVF treatment. If you do not take home a baby as a result of those cycles (and the transfer of any frozen embryos), 100 percent of the fee is refunded, preserving your resources for other family building options (some exclusions may apply).
- 100% Shared Risk Refund Guarantee for IVF and Donor Egg [Video]
- Read Sara and Kevin’s Patient Journey
At Shady Grove Fertility, we understand the financial considerations that go into the decision to begin—or continue—fertility treatment. As part of our efforts to make treatment more affordable, we participate with more than 30 insurance providers. While many patients have some form of insurance coverage for treatment, or live in a location that has coverage provided by mandate, we recognize that there are many without sufficient coverage or insurance benefits. With that in mind, SGF developed additional financial programs to help ease the cost of treatment.