Knowing that 20 percent of women who struggle with infertility have an underlying uterine condition or anomaly, you may wonder: how does my uterus affect my fertility?
Rest assured, a uterine diagnosis won’t always lead to challenges with getting pregnant or eventual pregnancy complications. We asked SGF California’s Dr. Alexander Quaas to shine a light on how to test the uterus for various uterine anomalies and conditions and what they mean for fertility.
Five uterine anomalies and what they mean for fertility
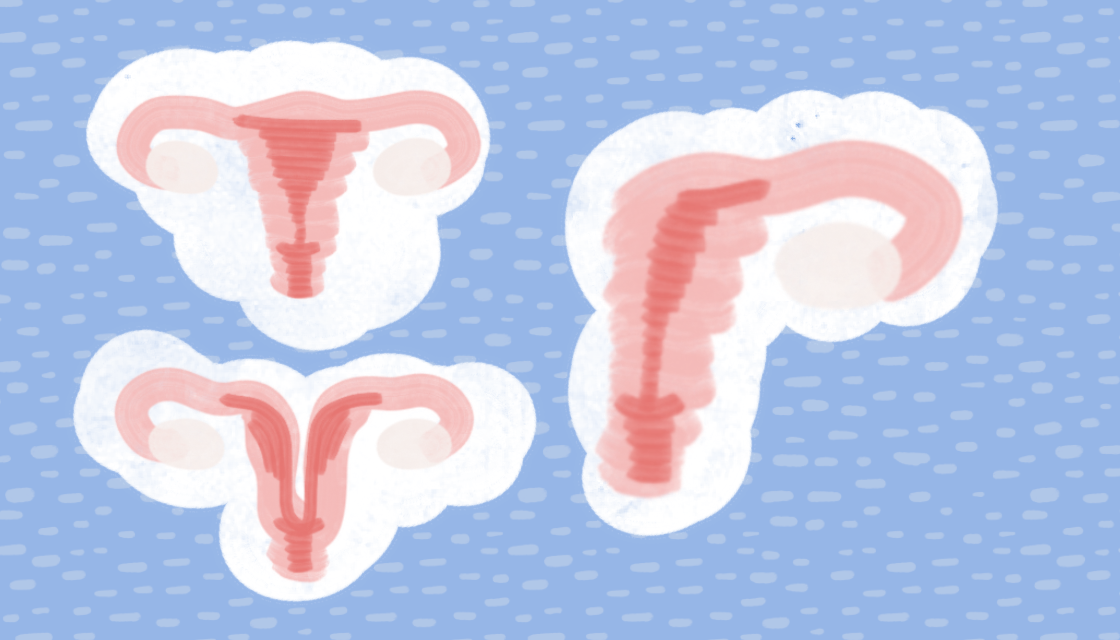
When anomalies form in utero and are present at birth, they are known as congenital. Some of these anomalies are classified as Müllerian anomalies, which affect up to 4 percent of women. So, what is a Müllerian anomaly?
“Think back to the early developmental stages of an embryo,” explains Dr. Quaas. “The entire female reproductive tract — the uterus, cervix, Fallopian tubes, and vagina — starts as two Müllerian ducts. But when the development of Müllerian ducts is disrupted, anomalies become present in the reproductive tract. Oftentimes, women are not aware of the anomalies until puberty or when they experience reproductive challenges.”
1. Septate Uterus: A Wall of Tissue
A uterine septum is a type of barrier in an otherwise normal-looking uterus. It occurs when the inside of the cavity is segmented by a wall of tissue that extends partially or for the entirety of the cavity of the uterus.
“A septum usually doesn’t have a flowing blood supply, making it very difficult for an embryo to successfully implant there,” says Dr. Quaas. “This may lead to an early pregnancy loss.”
For patients with recurrent miscarriages, doctors often perform an exam called a hysteroscopy to see the inside of the uterus. If there is a septum, doctors can remove it during that procedure, which can help women carry babies to term.
2. Arcuate Uterus: Normal Variant
An arcuate uterus is one of the milder Müllerian anomalies oftentimes characterized by a slight indentation at the top of the uterus, where it is otherwise rounded like the bottom of a pear.
“Indentations can be so minor that an arcuate uterus is practically normal,” explains Dr. Quaas.
The arcuate uterus is not known to be associated with pregnancy complications and infertility.
3. Unicornuate Uterus: Half a Uterus
A unicornuate uterus is one of the rarer congenital Müllerian anomalies and occurs when only half of the uterus has formed.
“If you’re thinking the anomaly sounds like unicorn, that’s no coincidence,” explains Dr. Quaas. “Having only half of a uterus means that the uterus is smaller in size than normal and has only one Fallopian tube, earning this anomaly the nickname of a ‘single-horned uterus.’ A variation of a unicornuate uterus also includes a rudimentary horn resulting from the disrupted development of a Müllerian duct.”
Women with a unicornuate uterus run the risk of complications including recurrent miscarriages, preterm labor, and ectopic pregnancies. Unicornuate uteruses come in many variations, so it is important to understand the physiology of the uterus.
4. Uterine Didelphys: Two Separate Uteruses
A uterine didelphys is when someone has two separate uteruses. When the Müllerian ducts don’t fuse together properly during development, they may grow into two separate organs.
“Someone with a didelphys does not necessary have an issue carrying a pregnancy to term as long as the uterus carrying the pregnancy is close to normal size,” shares Dr. Quaas.
While this condition is rare, women often have successful pregnancies.
5. Bicornuate Uterus: Heart-Shaped Uterus
Another congenital abnormality is a bicornuate uterus, or heart-shaped uterus. A normal uterus will resemble a pear shape. With a bicornuate uterus, there is an indent at the top of the organ, leading to the condition’s nickname.
“Women with this condition aren’t as likely to experience infertility, but they can have a higher risk of preterm delivery or breech (babies),” explains Dr. Quaas. “Women experiencing complications simply don’t have enough space in their uterus.”
The size of the uterus determines how well it can carry a baby. Like a didelphys, women may live their lives unknowingly with this condition until trying to conceive or during pregnancy.
Common uterine conditions that can impact chances of conception
1. Uterine Polyps and Fibroids
Both polyps and fibroids are generally non-cancerous growths that take up space in the uterus affecting the ability for an embryo to implant and grow. Polyps are an overgrowth of the endometrial lining and fibroids are smooth muscle tumors of the uterus.
What does this mean for chances of conception?
“These [polyps and fibroids] obstructions in the uterus are the most common on our list of uterine factors that can make the uterus less ideal for pregnancy,” explains Dr. Quaas.
Once removed, women can continue to try to conceive on their own or by using fertility treatment such as intrauterine insemination (IUI) or in vitro fertilization (IVF).
What are the symptoms?
Dr. Quaas explains that some women with uterine polyps and fibroids do not experience any symptoms, while others may have abnormal bleeding, cramping or pain.
How is this condition treated?
While some women with smaller masses can conceive, polyps and fibroids often need to be surgically removed. For polyps, this can always be done hysteroscopically, in other words by using a camera inserted into the uterus with a vaginal approach. For fibroids, it can be done using the hysteroscopy method if the fibroid is located inside the uterine cavity. Fibroids inside the uterine cavity have the highest impact on implantation and should always be removed. Fibroids that are located away from the uterine cavity do not always have to be removed. A decision on whether to remove fibroids and proceed with a “myomectomy” is an individual decision made on a case-by-case basis, considering the risks and expected benefits of the procedure.
2. Adenomyosis
Adenomyosis occurs when endometrial tissue grows inside the muscle of the uterus rather than lining the uterine walls. It is like endometriosis in that adenomyosis is also an estrogen responsive condition.
What does this mean for chances of conception?
Most cases of adenomyosis are present in women who are in their 40s and 50s. Nearly 70 to 80 percent of women who undergo a hysterectomy for adenomyosis fall within this age bracket. Age is one of the main indicators of a woman’s fertility, with sharp declines at ages 35 and older.
What are the symptoms?
Adenomyosis can be difficult to diagnose for two reasons: one, because the condition frequently co-exists with fibroids, and two, because symptoms closely resemble those of endometriosis. Common symptoms include:
- Heavy or prolonged menstrual bleeding
- Severe and sharp menstrual cramps
- Chronic pelvic pain
- Painful intercourse
How is this condition treated?
Adenomyosis tends to go away after menopause. For women who aren’t approaching menopause, treatment options include:
- Anti-inflammatory drugs
- Hormone medications
- Hysterectomy
3. Asherman’s Syndrome and Scar Tissue
Asherman’s syndrome is the presence of scar tissue, or adhesions, in the uterus.
What does this mean for chances of conception?
“Asherman’s syndrome can also impact the ability for an embryo to implant in the uterus,” says Dr. Quaas. “For many women, the formation of adhesions in the uterus is most frequently seen after surgical procedures including a dilation and curettage (D&C), fibroid removal surgery, or due to the occurrence of a retained placenta after the delivery of a baby.”
What are the symptoms?
Symptoms for Asherman’s Syndrome can vary from patient to patient and can include:
- light or absent periods
- pain during the time that menstruation should be occurring (often there is no menstrual blood because adhesions prevent it from exiting the uterus)
- miscarriage
How is this condition treated?
Women with a significant presence of scar tissue in the uterus are mostly frequently treated through a surgical procedure where the scar tissue is removed.
4. Hydrosalpinx
“A hydrosalpinx is a blocked Fallopian tube that becomes dilated and filled with liquid,” explains Dr. Quaas. “This liquid can spill into the uterus and affect the protein expression in the uterine lining.”
A hydrosalpinx often occurs due to a previous infection such as chlamydia or gonorrhea, a ruptured appendix, or due to endometriosis.
What does this mean for chances of conception?
The presence of a hydrosalpinx has been found to decrease implantation rates and increase the occurrence of miscarriage.
What are the symptoms?
Symptoms vary, with some experiencing recurrent abdominal pain, while others will not have any symptoms.
How is this condition treated?
To prevent the liquid found in the hydrosalpinx from spilling into the uterus, it is recommended that the affected Fallopian tube be tied off at the entry point or be removed completely. A woman with both tubes that become damaged may need fertility treatments such as IVF.
How to diagnose uterine conditions
If uterine anomalies or conditions are suspected, patients will generally undergo one of three tests to confirm a diagnosis:
- Hysteroscopy: A surgical procedure that allows a physician to look inside the uterus to investigate the source of abnormal uterine bleeding, or a cause of infertility or miscarriages.
- Sonohysterogram: An ultrasound-based test used to evaluate the uterine cavity. During this study, a small volume of saline is instilled into the uterus while an ultrasound is performed. This allows a physician to determine if fibroids or polyps are protruding into the uterine cavity, potentially disrupting embryo implantation.
- Hysterosalpingogram (HSG): An x-ray and dye test that a physician will use to detect several kinds of issues, such as polyps, fibroids, or scarring in the lining of the uterus, and blockages in the Fallopian tubes.
You may have heard about women’s experiences with HSGs. SGF Nurse Practitioner, Ursula “Fallopian Tube Queen” Rocha shares what to expect at your HSG.
Schedule an appointment
If you have a known uterine condition that may be impacting your ability to conceive, we recommend a consult to see a fertility specialist. To learn more, or to schedule an appointment, please call 1-877-971-7755 or complete this brief form.
Medical contribution by Alexander Quaas, M.D., Ph.D.
Alexander Quaas, M.D., Ph.D., is board certified in obstetrics and gynecology (OB/GYN) as well as reproductive endocrinology and infertility (REI). Dr. Quaas completed his residency in OB/GYN at Brigham and Women’s / Massachusetts General Hospital in the Harvard Integrated OB/GYN Residency Program. He completed his REI fellowship at the University of Southern California in Los Angeles.
Editorial note: This article was originally published in October 2016, and has been updated for accuracy and comprehensiveness as of January 2024.