Medical Contribution by Naveed Khan, M.D.

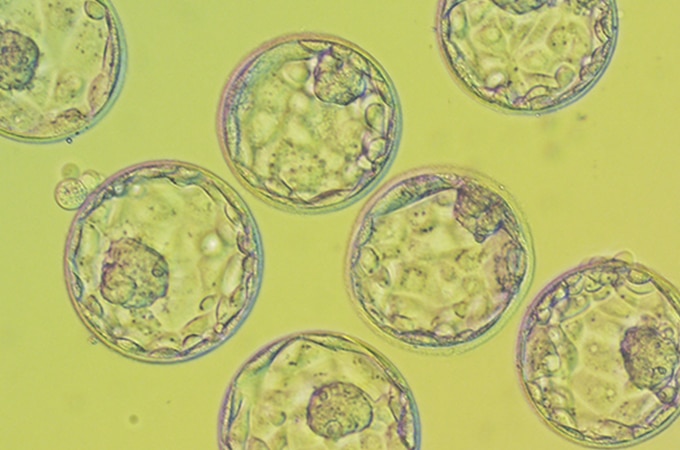
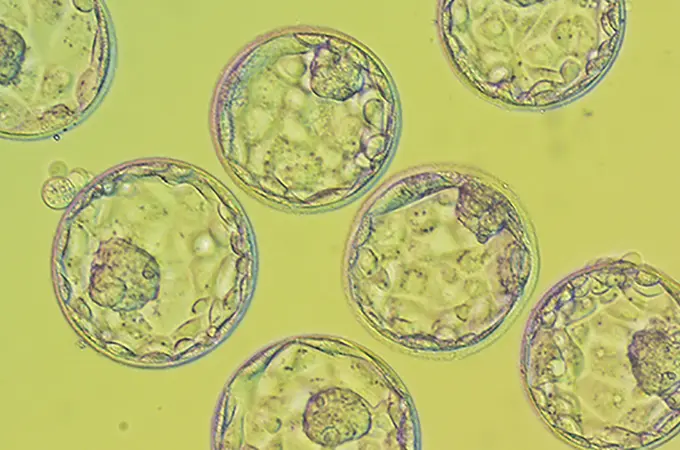
In the past decade, one of the greatest advancements in fertility treatment has been vitrification. Vitrification is a flash-freeze technology used for freezing eggs and embryos for the purpose of using them at a later date. While cryopreservation had existed to fulfill the same purpose for many years, the process frequently resulted in the formation of ice crystals in the eggs and embryos, often rendering them unusable. Vitrification’s flash-freeze technology, though, has remarkably advanced the freezing process and corrected earlier flaws. “One of the largest benefits of using vitrification has been increasing the success rates when using frozen embryo transfers (FET), as vitrification has doubled the ongoing pregnancy rate per embryo transfer in the past five years,” says Dr. Naveed Khan of Shady Grove Fertility’s Leesburg, Virginia office.
In order to undergo a frozen embryo transfer though, you must first perform a fresh in vitro fertilization (IVF) cycle. Oftentimes, there may be additional unused embryos from a fresh cycle. This is where vitrification can be used to preserve the embryos for a later date and a patient can eventually return for a frozen embryo transfer cycle.
Who will utilize a frozen embryo transfer (FET)?
A frozen embryo transfer (FET) can be performed by any patient who has frozen leftover embryos from a fresh autologous IVF or donor egg cycle. The use of frozen embryos may come immediately following an unsuccessful fresh cycle, or, for patients who were successful with their fresh cycle, a FET can be used at a later date to have additional children.
What are the benefits of FET in comparison to performing another fresh (stimulated) cycle?

FET is often a good choice over completing another fresh IVF cycle when a patient has frozen embryos to use, as they have a lower cost (see the financial programs section below) and there is no need to have an egg retrieval. “Additionally, the date of the frozen embryo transfer is much more predictable than that of a fresh cycle, as you do not have to wait for the embryos to develop and mature. A FET cycle works much better in terms of planning around the transfer itself,” explains Dr. Khan.
What are the success rates for IVF with FET compared to that of a fresh cycle?

The success rates for FETs have doubled in the past five years, with an ongoing pregnancy per embryo transfer rate equal to – or sometimes even greater than – that of fresh transfers. In 2013, women under 35 had a 51% ongoing pregnancy rate per frozen embryo transfer. In comparison in 2013, women under 35 had a 48% ongoing pregnancy rate per fresh embryo transfer. FET cycles had a slightly higher success rate than fresh cycles, which can happen due to the presence of more balanced hormones and the fact that only high-quality blastocyst-stage embryos are being used for FETs.
How long does a FET cycle take?
A patient will contact our office with her desire to begin a frozen cycle. Her records will be reviewed to ensure that her prescreening is up-to-date. This can include – but is not limited to – infectious disease bloodwork, pap smear, an updated mock embryo transfer (to accurately measure and map your uterine contours), consents, and an injection review.
Prior to the frozen cycle beginning, most patients will be on a cycle/month of oral contraceptives. Soon after, the patient will come in for their first monitoring appointment, which is a baseline evaluation before the medications are started. Patients will then begin sequential injections of estrogen to build the uterine lining. Mid-cycle, the patient will have to have a ‘lining check,’ to ensure that the uterine lining has thickened. Patients will then be instructed to add in progesterone. A frozen embryo transfer date will be confirmed and then the patient will return for her actual frozen transfer. Approximately two weeks after the transfer, the patient will have a blood pregnancy test (known as the beta hCG).
What types of medications are required for FETs?
“Unlike in a fresh IVF cycle, medications to stimulate the ovaries are not needed for a FET,” says Dr. Khan. “Instead, supplemental estrogen and progesterone are the chief medicinal components of a FET cycle.” Estrogen will be given in the form of an injection every three days to build the uterine lining. Progesterone will be administered in the form of an injection every day as instructed after the mid-cycle ‘lining check,’ to ensure that the uterine lining has thickened, increasing the chances of implantation for the embryo. The estrogen and progesterone supplements will continue to be taken through the point of the patient’s beta hCG, with the progesterone continuing for up to eight weeks after the hCG. Once the pregnancy is confirmed though, the progesterone is taken as a vaginal suppository instead of an injection.
What financial programs are available for FETs?
For patients who have frozen embryos available for transfer, they may be eligible for the Shady Grove Fertility Shared Risk 100% Refund Program for FET. Once a patient is approved for this program, they will pay a flat-fee and then receive unlimited FET cycles while in the program, for as many frozen embryos as that patient may have. They can only use embryos that were vitrified at Shady Grove Fertility though, not embryos from other locations. In terms of program completion, a patient has the following possible outcomes: they will have a successful pregnancy and delivery; they will withdraw from the program at any time and receive a full refund; or they will use all of the embryos that are available without conceiving and then receive a full refund as well (some exclusions apply).
What are additional benefits of FET cycles?
While FETs have been beneficial in increasing the chances of conception per egg retrieval (when including fresh and frozen embryo transfers), they have also helped to change the treatment process in other areas of reproductive medicine.
On a large scale, FETs have helped to widen the practice of elective single embryo transfer (eSET), resulting in safer singleton pregnancies. In the past, multiple embryos were often transferred because technology was not as strong and IVF was not as successful. “Advances in technology and the embryo culture environment have resulted in the ability for embryos to develop to the blastocyst stage, two days longer than in the past. As a result, embryologists can now more accurately identify which embryos have the highest quality, making possible the selection of a single embryo that is a likely candidate for success, which has significantly decreased the risk of a multiple pregnancy,” Dr. Khan states. “In conjunction with this, vitrification allows additional embryos to be safely preserved. So even in the event that an eSET cycle is unsuccessful, patients may have additional embryos available for future FETs and do not have to feel the need to transfer multiple embryos initially.”
Another lesser known benefit of FETs is the ability to freeze all of the embryos for a later transfer. This is commonly seen when patients are choosing to genetically test the embryos or when an increased progesterone level is found in the patient. SGF’s research team has extensively studied rising progesterone levels and their effect on the chances of a successful pregnancy. Studies have shown that women who have higher progesterone levels at the time of their ‘trigger shot’ before the egg retrieval have a decreased chance of implantation and pregnancy. Dr. Khan says, “As a result, women who are found to have these prematurely rising progesterone levels now have the option to freeze all of their embryos. This allows the progesterone to return to more normal levels, providing the embryo with the best possible environment for implantation.” This two-step process of freezing the embryos following the fresh IVF cycle and then transferring during a FET cycle will allow a patient to have the best chance for a successful pregnancy. While this option only impacts a small percentage of our IVF patients, it depicts yet another way in which this newer technology has helped to improve our patients’ chances of conception.
Frozen Embryo Transfers are Changing the Face of Fertility Treatment
Since the advent of vitrification technology, FET cycles have represented one of the most revolutionary changes in fertility treatment. These cycles provide patients with additional options, whether it’s because they have an unsuccessful cycle or because they want to come back in a few years to further grow their family. FET cycles can also be beneficial because they are easier to plan around and an additional egg retrieval will not be needed. Additionally, FETs have helped to increase the ability for patients to have singleton pregnancies through eSET or to provide the ‘freeze-all’ option for patients. In all of these instances, FETs represent a way to extend fertility treatment. Freezing or suspending these embryos in time preserves them at their current quality, providing patients with an optimal chance for future success.
For more information or to schedule an appointment with one of our physicians, please speak with one of our New Patient Liaisons by calling 888-761-1967.